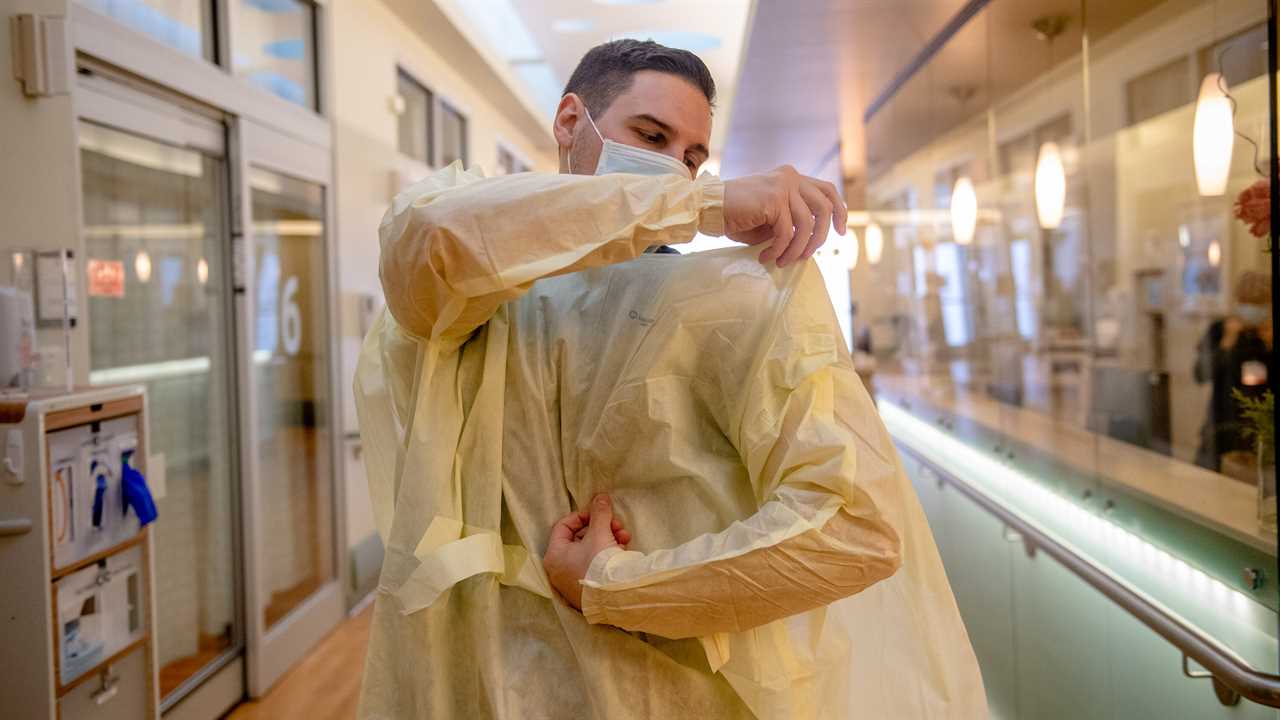
As Americans celebrate the rollout of a coronavirus vaccine, many of the doctors and nurses first in line for inoculation say a victory lap is premature. They fear that the optimism stirred by the vaccine will overshadow a crisis that has drawn scant public attention in recent months: the alarming shortage of personal protective equipment, or P.P.E., that has led frontline medical workers to ration their use of the disposable gloves, gowns and N95 respirator masks that reduce the spread of infection.
At St. Mary’s Medical Center in Duluth, Minn., health care workers who treat Covid-19 patients are required to reuse their tightfitting respirator masks up to six times before throwing them away. Although soiled N95s are sterilized each day with ultraviolet light, Chris Rubesch, 32, a cardiac nurse, says the masks invariably sag after two or three shifts, leaving gaps that can allow the virus to seep through. “Our days are filled with fear and doubt,” Mr. Rubesch said. “It’s like driving a car without seatbelts.”
Many of the shortages are the result of skyrocketing global demand, but supply chain experts and health care providers say the Trump administration’s largely hands-off approach to the production and distribution of protective gear over the past nine months has worsened the problem. That has left states and hospitals to compete for limited supplies. Price gouging has become the norm, and scores of desperate institutions have been duped into buying counterfeit products.
President Trump has made only sparing use of the Defense Production Act, a Korean War-era law that allows federal agencies to coordinate the distribution of scarce goods and force companies to prioritize government orders. The D.P.A. can also provide grants to companies that need help ramping up production.
“It’s been an absolute free-for-all, and the federal government has failed to provide any meaningful leadership,” said Scott LaRue, the president of ArchCare, a nonprofit operator of nursing homes in New York State.
Although the vaccine will help protect health care workers from falling seriously ill with Covid-19, it is unclear how long that protection will last and whether vaccinated people will still be able to transmit the virus to others — including patients of all stripes who seek their care.
At Community First Medical Center in Chicago, Kathy Haff, a registered nurse, said employees there are often given N95 masks that don’t fit their faces. She blamed the shortage of appropriate gear for the coronavirus deaths of three nurses at her hospital this past spring and summer.
“Things are going to get worse before they get better, especially if we don’t have enough P.P.E.,” Ms. Haff said.
With the White House largely disengaged from the crisis, medical workers, supply chain specialists and public health experts are urging President-elect Biden to make good on his campaign promises to use the Defense Production Act to boost domestic manufacturing of personal protective equipment, test kits, vaccines and the medical supplies needed to immunize hundreds of millions of Americans. They are also hoping the incoming administration will take over the distribution of scarce goods and put an end to profiteering and the mad scramble for P.P.E. that has pitted states and deep-pocketed hospital chains against nursing homes and small rural hospitals.
“This is not a time for complacency from the federal government,” said Stanley M. Bergman, the chief executive of the medical gear distributor Henry Schein. The community clinics, cancer care centers and family care practitioners his company serves, he said, are still hampered by an inability to obtain masks and gloves. “We need bold action,” he said.
Hospital purchasing agents say they are facing an unparalleled shortage of single-use nitrile gloves — one of the most important items for reducing the spread of infectious pathogens — with prices soaring to $300 a case from $30 before the pandemic. Get Us PPE, a volunteer organization that connects health care facilities to available protective gear, says requests for help have more than tripled in the first half of December compared with the same period last month. Nearly 90 percent of the frontline workers the group surveyed across the country say they are repeatedly reusing masks designed for single use.
The pandemic has exposed flaws in freewheeling distribution system that enables hoarding by wealthy hospital chains and a global supply network overly reliant on overseas manufacturers. This was evident in the early months of the pandemic, when transcontinental flights that ferry Asian-made medical gear to the United States were largely frozen. And the crisis grew worse as China turned off the export spigot and commandeered its mask factories for domestic use.
Latest Updates
- A C.D.C. panel says frontline workers and people over 74 should get vaccines next.
- Thailand announces its biggest outbreak to date, linked to a shrimp market.
- The official leading Operation Warp Speed pins the blame for vaccine shortfalls on an administrative error.
For nearly two decades, Mike Bowen has heard politicians make promises to address the nation’s supply chain problems only to be disappointed. As the owner of Prestige Ameritech, an N95 mask manufacturer in Texas, Mr. Bowen has been warning federal officials about the country’s reliance on overseas factories, which make more than 90 percent of the world’s medical face masks.
In early January, when the coronavirus first emerged in China, he wrote to the Department of Health and Human Services offering to ramp up production. The offer, he said, fell on deaf ears.
His letter became public in April after Dr. Rick Bright, then the director of H.H.S.’s Biomedical Advanced Research and Development Authority, included it in a whistle-blower complaint. Dr. Bright had filed the 89-page complaint with the Office of Special Counsel, not long after he was outsted from his job by the White House amid a dispute over an unproven coronavirus treatment pushed by President Trump.
Alarmed by the federal government’s lack of response but determined to pitch in, Mr. Bowen invested millions of dollars to build more machines and he hired 200 additional workers, allowing Prestige Ameritech to increase production to six million masks a month, up from 75,000 in March. “I did it all without a penny of government help,” said Mr. Bowen, whose company is one of the country’s largest domestic mask producers.
By next spring, he said, his factory will be producing 10 million masks a month. Still, Mr. Bowen worries he will be saddled with unsold product. “A few months ago my phone was literally ringing all the time and I was getting thousands of emails per day,” he said. “Right now my phone just isn’t ringing that much.”
The problem, Mr. Bowen said, is that the hospitals that were once so eager to purchase his N95 masks have begun buying cheaper products from China, which have become more widely available in the months since Beijing brought its pandemic under control.
Luis Arguello Jr., the vice president of DemeTech, a surgical suture manufacturer in Florida that jumped into the mask business in the spring, says he has also seen a similar slump as state officials seeking to replenish their stockpiles buy foreign-made goods with federal money. “We have product and we have capacity, but they’re not really buying it,” said Mr. Arguello, whose company is now making 100 million masks a month. He is concerned that hospitals swayed by the comparatively low cost of Chinese masks might end up buying inferior products.
Public health experts say solving this crisis will be a heavy lift for Mr. Biden, but they have been encouraged by his words, and by the experts he has appointed to his Covid-19 advisory board. One of the appointees, Dr. Bright, the federal scientist ousted from his job, has been discussing the problem with domestic manufacturers, supply chain experts and state officials.
Dr. Bright is troubled by what he has heard, he said, including reports of millions of test kits gathering dust in a warehouse because of a collection swab shortage and nursing homes unable to use rapid-result test machines provided by the federal government because they arrived without instructions. “There is not a lot of coordination out there right now, and lots of community confusion and chaos,” he said.
The incoming administration, he said, is exploring ways to take over the distribution of testing supplies and medical gear. They are also seeking to create financial incentives and “buy American” policies to boost the handful of domestic companies that make P.P.E., he said. Mr. Biden would not hesitate to embrace the Defense Production Act, Dr. Bright said, though he did not provide details on how it would be employed.
Industry executives say the only way to guarantee the United States has a reliable supply of high-quality masks and other medical gear is to recognize the sector as essential for national security, similar to the Pentagon’s approach for ensuring companies that make fighter jet components and military uniforms remain viable even in peacetime.
That could mean providing loans and subsidies to domestic companies, mandating that state and national stockpiles acquire American-made medical products, and perhaps requiring hospital chains to source some of their supplies from homegrown manufacturers.
“Masks are not a big spend,” Mr. Bowen said. “The whole damn market is less than $150 million.”
Dan DeLay, who oversees procurement at CommonSpirit Health, the nation’s second-largest nonprofit hospital chain, said the pandemic had opened his eyes to the importance of domestic supplies. But, he said, it can be challenging to convince hospital executives to buy American-made protective gear, which can cost 40 percent more than goods manufactured overseas. “If we’re serious about domestic manufacturing, we’re going to have to make a serious investment that is sustained over the long haul in case something like this happens again,” he said.
For now, the legions of exhausted health care workers are focused on getting through the current crisis. Mary Turner, president of the Minnesota Nurses Association, said the monthslong shortages had left many members feeling unappreciated and angry. Ms. Turner, who is also an I.C.U. nurse at North Memorial Medical Center in Robbinsdale, Minn., recalled the days before the pandemic, when nurses were given an N95 mask for each patient. These days, she frequently hears from nurses forced to use the masks up to 10 times, “or until they fall off their faces,” she said.
Despite her optimism that a Biden administration will be different, she is weary of political leaders who lionize medical workers as frontline warriors but do little to help keep them safe, she said.
“The total disregard for our safety has been unconscionable,” she said. “They call us heroes but we’re not being treated like soldiers at war because if we were, the federal government would make sure we have everything we need.”
Did you miss our previous article...
https://trendinginthenews.com/usa-politics/stimulus-deal-provides-economic-relief-for-now






