SEPSIS is the primary cause of death from infection around the world, claiming around 40,000 lives in the UK each year.
That’s more than bowel, breast and prostate cancer combined. Here’s all the information you need.
What is sepsis?
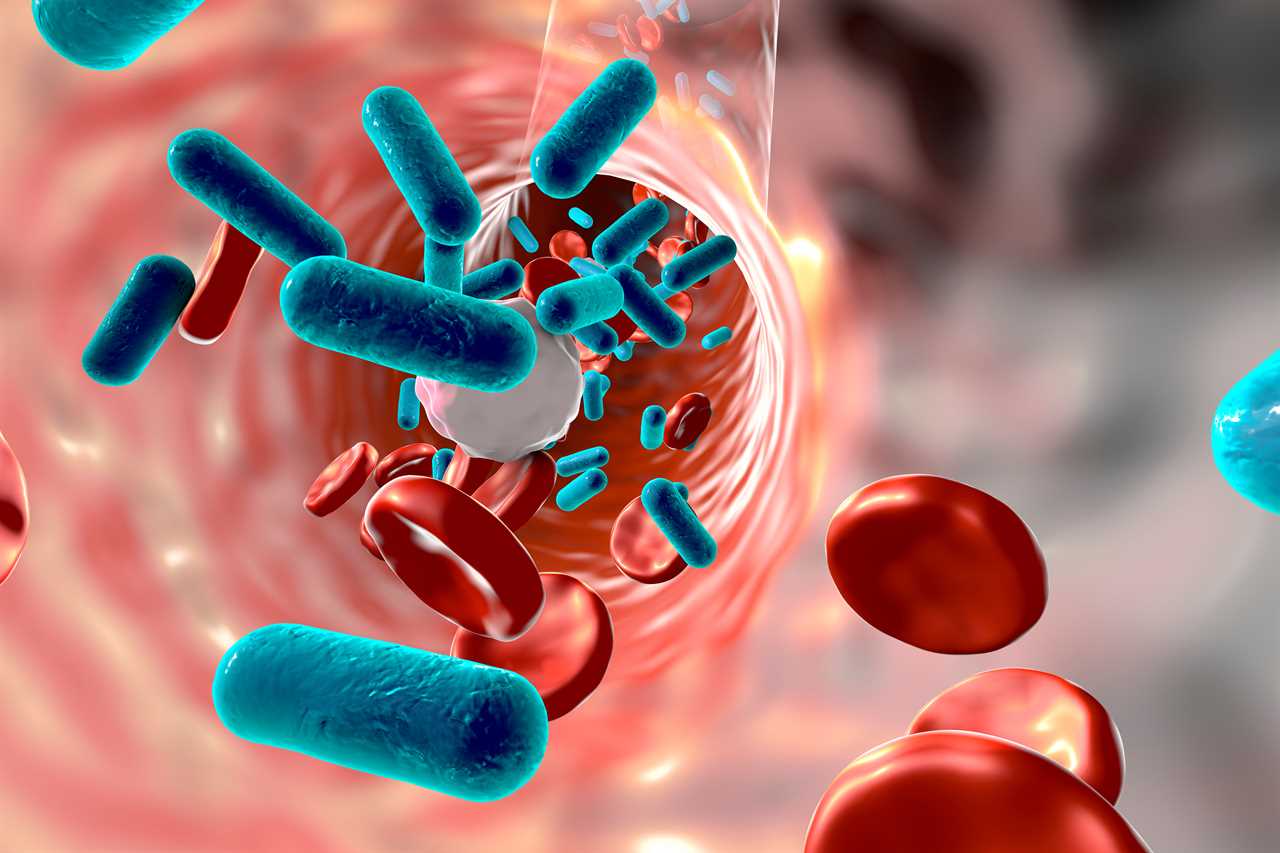
The condition is always triggered by an infection.
It is not contagious and cannot be passed from person to person.
Most often the culprit is an infection we all recognise – pneumonia, urinary infections (UTIs), skin infections, including cellulitis, and infections in the stomach, for example appendicitis.
Typically, when a person suffers a minor cut, the area surrounding the wound will become red, swollen and warm to touch.
This is evidence the body’s immune system has kicked into action, releasing white blood cells to the site of the injury to kill off the bacteria causing the infection.
The white blood cells and platelets form blood clots in the tissues around the cut.
Blood vessels swell to allow more blood to flow, and they become leaky, allowing infection-fighting cells to get out of the blood and into the tissues where they are needed.
This causes inflammation, which appears to us as the red, warm swelling.
When sepsis happens, this system goes into overdrive.
The inflammation that is typically seen just around the minor cut, spreads through the body, affecting healthy tissue and organs.
The immune system – the body’s defence mechanism – overreacts and the result is it attacks the body.
It can lead to organ failure and septic shock, which can prove fatal.
Bacteria, viruses, fungi and parasites can all trigger sepsis – though the most dangerous culprit is bacteria.
In developing nations, the condition remains a leading cause of death.
Known by its colloquial name “blood poisoning”, sepsis is also often referred to as a “flesh-eating disease”.
What is septicaemia?
The terms sepsis and septicaemia both refer to a blood infection that’s typically caused by bacteria.
Even though the definitions are closely related, there are some small differences.
Sepsis occurs when your body reacts to a severe infection, whereas septicaemia is the name of the infection itself.
The NHS explains: “Sepsis can affect multiple organs or the entire body, even without blood poisoning or septicaemia.
“Sepsis can also be caused by viral or fungal infections, although bacterial infections are by far the most common cause.”
What are the three stages of sepsis?
Sepsis affects the body in three distinct stages.
Stage One
An infection invades a specific part of the body – pneumonia affects the lungs, for example – triggering the immune system into action.
The germs and toxins produced by the bacteria or virus leave the original site of infection and enter the bloodstream.
This causes the inflammatory response known as SIRS (systemic inflammatory response syndrome).
Stage Two
Individual organs throughout the body become affected and begin to deteriorate.
In severe cases, this can lead to organ failure.
Stage Three
More than one organ stops functioning, and the patient experiences cardio-circulatory failure that leads to a sudden drop in blood pressure.
This is known more commonly as septic shock.
Who is most at risk from sepsis?
Sepsis is a condition that fails to discriminate – it can affect old and young, those who lead healthy lives and those who don’t.
As with many life-threatening illnesses, the most vulnerable are newborns, young children and the elderly, as well as anyone with a weakened immune system.
Though it can affect us all, men are more susceptible than women, black people are more at risk than white, and the very young and very old are more likely to be affected than any other age group.
Those people battling diabetes, Aids, kidney or liver disease are also at greater risk due to their weakened immune systems.
And pregnant women and people who have suffered severe burns or physical injury are more likely to fall victim to the life-threatening condition.
What are the signs of sepsis you should never ignore?
If you, a loved one, or in the case of medical professionals their patient, feels “severely sick”, doesn’t appear to be themselves and shows any of the following symptoms, sepsis should be suspected:
- weakness
- loss of appetite
- fever and chills
- thirst
- difficult or rapid breathing
- rapid heart rate
- low blood pressure
- low urine output
If a person is suffering these symptoms and they are thought to have suffered an infection – pneumonia, abdominal infection, urinary infection, or a wound – sepsis is a likely cause.
What treatment is available and can you prevent sepsis?
If you suspect you or a loved one are suffering sepsis it must be treated as a medical emergency.
Think of the reaction you would have to a heart attack, stroke or major car crash – dial 999.
A person’s chances of surviving sepsis are highly dependent on their getting medical intensive care as soon as possible.
The longer it takes to receive medical care the more likely it is a patient will die.
Patients who appear to have a least one sign of sepsis must be seen by a senior doctor within 60 minutes, an NHS watchdog has said.
Given it is a condition triggered by an infection, preventing that initial infection can prevent sepsis.
But how can we prevent the many infections out there from infecting us?
Vaccinations
Vaccinating children against various illnesses can help protect not only them but also their grandparents.
The youngest and oldest in society are at greatest risk of a strain of bacteria known as pneumococcus bacteria.
This is the vicious strain responsible for triggering pneumonia, middle ear infection and meningitis, and can ultimately lead to sepsis.
Vaccinating babies and young children results in “herd immunity”, preventing infections from taking hold within communities, and spreading rapidly through the population.
Antibiotic use must be restricted
Antibiotic resistance is a growing health concern the world over.
The excessive use of the drugs for decades has led to a sharp increase in the number of bacteria that have mutated and developed the resist the medication.
The implication is that common and typically minor infections could become killers once more.
In order to prevent this from happening, it is vital that antibiotics are only used when absolutely necessary – and that the right type of antibiotic is prescribed to tackle the right infection.
Furthermore, it is important that the drugs are only prescribed for a limited period of time – taking them for prolonged periods of time can increase the risk of resistance building.
Wash those hands
Poor hygiene increases the risk of picking up infections.
And the risk of poor hygiene is more pronounced in areas where resources are lacking.
In these parts of the world, day-to-day things like giving birth and treating wounds, that are taken for granted in more prosperous nations, can prove fatal.
Promotion of good personal hygiene, hand washing and making sure clean water is more widely available have the potential to save millions of lives, by lowering the risk of sepsis.
Is sepsis on the rise?
Sepsis is considered a bigger threat than meningitis.
The rise has prompted the head of the UK Sepsis Trust to urge all parents to be as vigilant for sepsis as meningitis.
The number of people developing sepsis is increasing, with around 123,000 cases each year in England.
An estimated 37,000 deaths are associated with the condition, according to NHS England.
And according to The UK Sepsis Trust every year in the UK 250,000 people are affected by sepsis; 52,000 people die because of it (1,000
which are children) and 60,000 suffer permanent, life-changing after effects.






