IT’S been a worrying week for the NHS with numbers of hospitalised Covid patients at an all time high.
Yesterday, an Essex trust called in the army after declaring a major incident, and patients are routinely being treated in ambulances outside hospitals, due to lack of space inside.

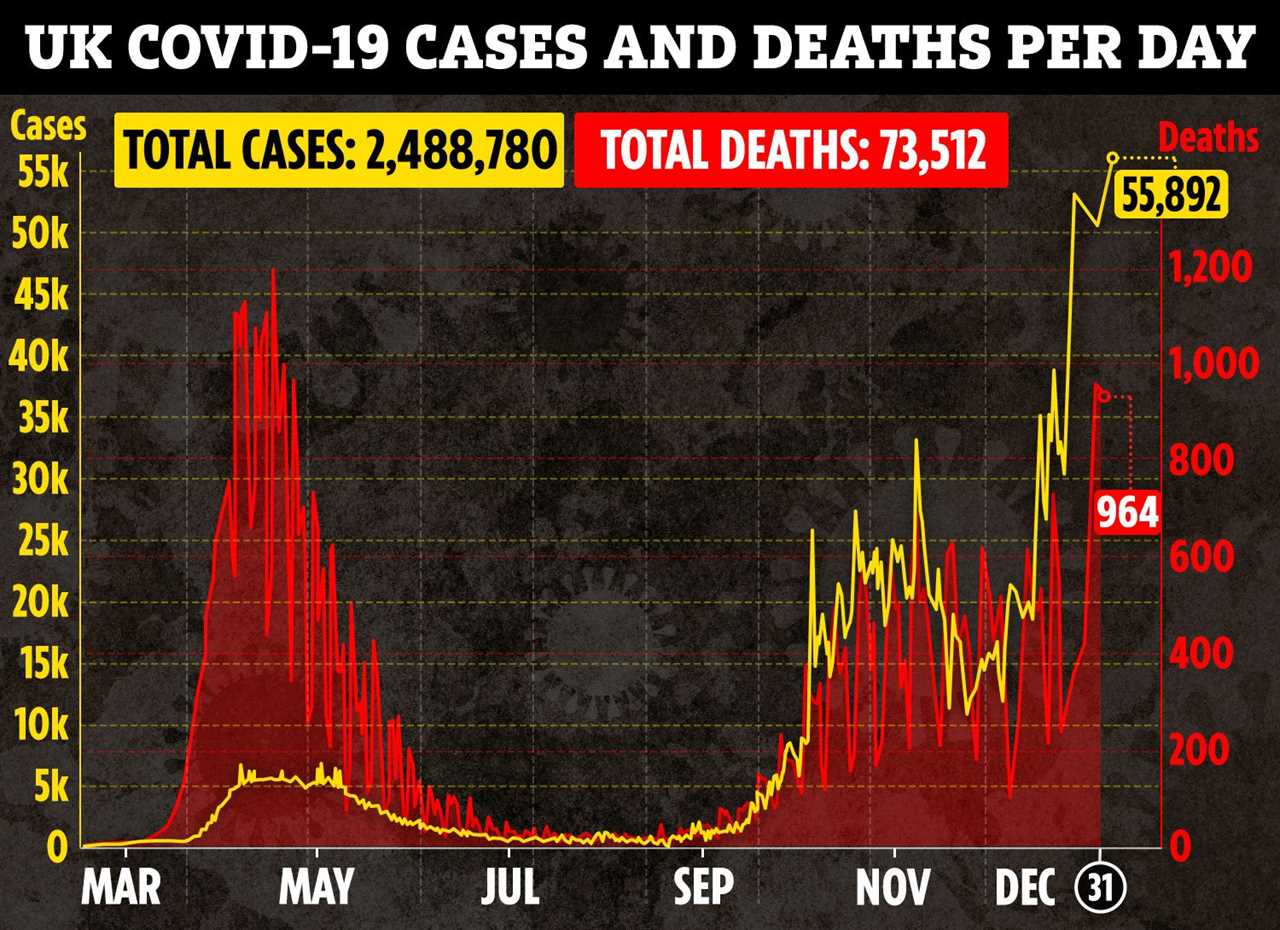
On Thursday, the Government said a further 964 people had died within 28 days of testing positive for Covid-19, bringing the UK total to 73,512. as hospital admissions go well past the April peak.
In an exclusive interview with the Sun, two frontline doctors reveal their tears over the latest Covid crisis and say the NHS – and its staff – are at breaking point.
Dr Pushpo Babul Hossain, a junior doctor working in South London, says: “I don’t think any health care system in the world is equipped to deal with a pandemic of this scale.
“We’re working all the hours we can and it’s absolutely draining. Sometimes, you don’t feel like you’re saving lives anymore.


“You’re on autopilot, you’re just firefighting, holding the fort until the next shift comes to rescue you.
“When we see the anti-vaxxers spreading nonsense and people refusing to wear masks, or obey the rules, it breaks our heart.
“How are we ever going to deal with the consequences of their actions? We really can’t.”
‘Haunted by memories of patient I couldn’t save’

Dr Pushpo Babul Hossain, 31, reveals the true horror of the Covid wards in her own words
She says: “Being a doctor should be a very rewarding profession but at the moment, we don’t have the time to feel anything.
We are having to deal with an unimaginable number of patients and doing so many extra hours, we’re in a non-stop, ‘eat, sleep, work, repeat’ cycle which is exhausting.
As a medical doctor on the Covid wards, I see patients who have been referred by A&E with suspected coronavirus infection.
Because we are so full, we’re only taking patients that desperately need oxygen.

Everyone else is told to go home, self-isolate, and monitor themselves for signs of breathlessness, chest tightness and chest pain.
As well as the Covid patients, here are some of those who were sick in the first wave but didn’t come in because of the pandemic and have now developed more serious complications of other diseases. It’s a recipe for disaster.
During the first wave, I had to fight to get a patient up to ITU and, just before my night shift ended, we finally got a bed.
I was relieved he was going into ITU and convinced we’d saved him.
The next morning, the bereavement office told me the gentleman had passed away, and I couldn’t believe it. He looked so good and was only in his 70s, so I really didn’t think we would lose him.
I had tried so hard for him and I remember I cried for a good 15 minutes. It still haunts me today.
But this time is worse. In the first wave, I was dealing with one case like that per day. Now it’s two to three cases per day and it’s getting worse.
Oxygen overload could mean system crashes
Never before have so many patients required oxygen at the same time and many NHS hospitals are old buildings which have not been built to deliver oxygen on such a large scale.
We do have the oxygen to supply to patients but what we don’t have is the capacity to provide it to all of them at the same time.
We are constantly reviewing all our patients to see who can come off oxygen, so we can reduce output.
If too much is being pulled out at once, there’s a risk that certain systems can collapse and cause a complete outage, meaning the hospital would have to be emptied out and people’s lives would be in danger.

The weekend before Christmas was the most stressful of my seven-year career because of the huge number of patients requiring urgent attention. We were just drowning – with two to three emergency calls coming at once.
I felt so scared and helpless.
My pager was bleeping non-stop and I was running around the hospital, dealing with two cardiac arrests and bed after bed of people suffering from lack of oxygen.
I did a vital protein level test on a heart patient suffering chest pains and it was five hours before I had time to read the results – which showed the level was 100 times what it should have been and required urgent treatment.
My heart sank. I remember thinking that this gentleman was my dad’s age and that could have been him lying there and receiving no treatment for five hours.
That weekend, I did three night shifts, back to back, without any breaks.
In a 13 hour shift, we’re allowed a 30 minute rest so we can sit down, eat something or just have a cup of coffee. I couldn’t do that.
On one shift, I didn’t sit down and drink water until 5am when my registrar marched me to the mess.
NHS at breaking point
The NHS is on its knees. There are so many sick patients, doubled with the fact that so many of our staff are off sick having caught the virus themselves, despite wearing all the correct PPE.
The new variant is more transmissible and a lot of my colleagues are coming down with Covid, so I don’t think the guidelines on protective equipment are adequate.
On one set of nights, two of my team of four came down with Covid.
The NHS has always been understaffed and staff levels are now lower than ever.
Everybody from clinical directors to medical students are putting in extra hours and we’re trying our best. But at the end of the day, we’re so tired.
I got married in October, in Bangladesh, and spent ten days with my husband, Taufiq, before coming back to the UK without him.
I’ve not seen him since and none of us know when we will next see our families because all our leave has been cancelled.

I work almost every day and a lot of doctors like me are volunteering to fill in the gaps that are left by our sick colleagues.
It’s no longer possible for doctors, health care workers and nurses to deal with this pandemic alone.
We all have to work together. The public has to understand that they need to play their part, we all need to play our part, to be able to fight this.
I understand that it is difficult, and frustrating and it’s taking a mental toll on people, because they’re being asked to stay at home. But this is the time when we need to think about the entire nation as a whole and protect the old and vulnerable.
Maybe you’re young and a Covid infection or a hospital stay of 10 days doesn’t affect you that much. But your 90-year-old gran can’t afford that.
And would you be able to forgive yourself if you lost your gran just because you were having a night out drinking at the pub? I don’t think so.
As much as the public think they need the NHS – the NHS now needs the public.”
‘We’re hailed as superheroes – but we break down too’
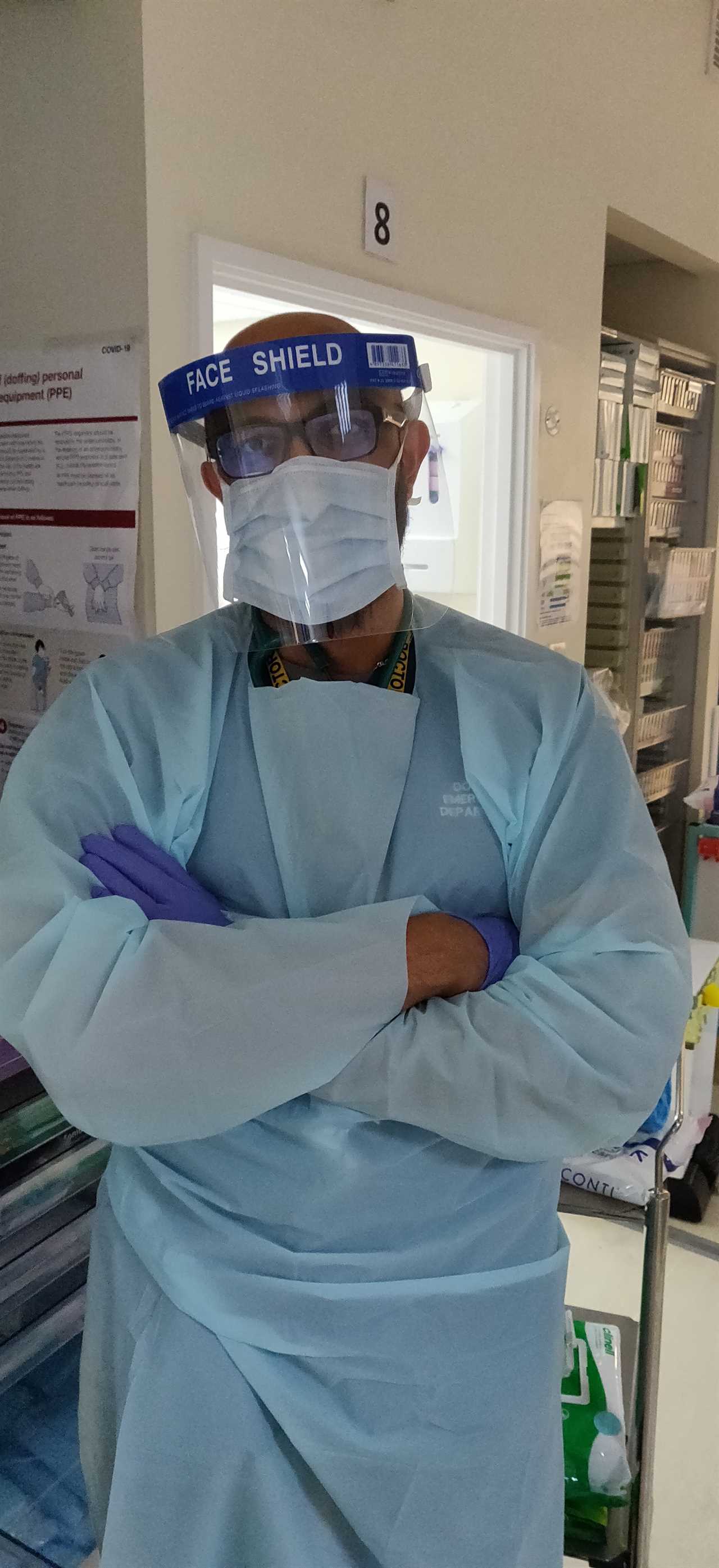
Dr Priyesh Patel, 31, is an A&E doctor who works at various London hospitals.
“I’ve just spent the last three days in A&E and the situation is terrible, with more and more people coming through the doors.
The numbers are higher than we experienced in March and April and it’s put so much pressure and strain on the whole hospital, not just the A&E department.
In A&E, we’re frequently running out of bed space and I’ve had to see seriously sick patients in ambulances, because they’ve been waiting for over four hours just to get inside the hospital.
In the resus department, where we battle to save the sickest patients, we can’t bring in any more because there’s no space.
The ICU departments are full which affects other departments, which have become Covid wards and it is trickling down all the way towards the paramedics.
I’ve seen people pass away in A&E and the number of people needing oxygen has significantly gone up, which is quite concerning because if we don’t have the bed space, we can’t provide supportive measures like ventilation.
Stress levels are so bad that the staff, even highly experienced doctors and nurses, can struggle to cope and emotions are running high.
People need to know we are human beings because what you see on the news is that we’re superheroes and it’s great to be thought of that way.
But we get very stressed, upset, emotional, we cry – and even have breakdowns.


Even I felt like crying at one point on Boxing Day because I was so stressed, I was tired, I was hungry, there were so many unwell patients to look after and more on the ambulances I was seriously concerned about.
I’ve lost track of how many 10 hour shifts I’ve done with a 15 minute lunch break, and it takes its toll.
In my department, it’s a common occurrence to see nurses and doctors get upset and even cry.
Also, doctors and hospital workers are now realising that they themselves can become sick, and that’s one of the scariest things.
When you work in a hospital, you get used to doing a job and you fix sickness in people. When it’s very busy, with so many things to do, you tend to see things as a tick box exercise and you mentally separate yourself from sick people.
But when your colleagues get really sick you immediately think ‘I could have caught Covid from that same sick patient – and now that doctor or nurse is on a ventilator.’
“In the first spike, in spring, there was the fear of the unknown and now we have a fear of the known.
“It feels scary because it’s more contagious, and more and more people are coming through the door.
“What people don’t realise is that, even before there was one case of Covid in the world our NHS was already struggling to cope. There were always bed shortages, and shortages of doctors and nurses, so the job was already difficult.
The pandemic means the situation has gone from difficult to worse.
But it’s important that we appreciate that we have such a great NHS system and we’re very lucky compared to other countries.
We have 1.3 million workers, for example, with a budget of £100billion,and we need to be very thankful for that.”






