BRITS now have two vaccine offerings that have been authorised to protect them from Covid-19.
Today the first Brit received the Oxford/AstraZeneca coronavirus vaccine as many more prepare to have the jab across the country.

Brian Pinker, a dialysis patient who describes himself as Oxford born and bred, received the jab at Oxford University Hospital at 7.30am.
Vulnerable people across the country started to receive the Pfizer/BioNTech jab in December, with their second doses also now taking place.
Boris Johnson pledged to vaccinate tens of millions within three months and said: “We can see how we are going to get out of this with great clarity now.”
Five thousand troops will begin “Operation Freedom” — with 530,000 Oxford/AstraZeneca jabs ready to roll out in the war on coronavirus.
Hospitals at six NHS trusts across London, Brighton, Oxford, Morecambe and Nuneaton will be the first to give the vaccine.
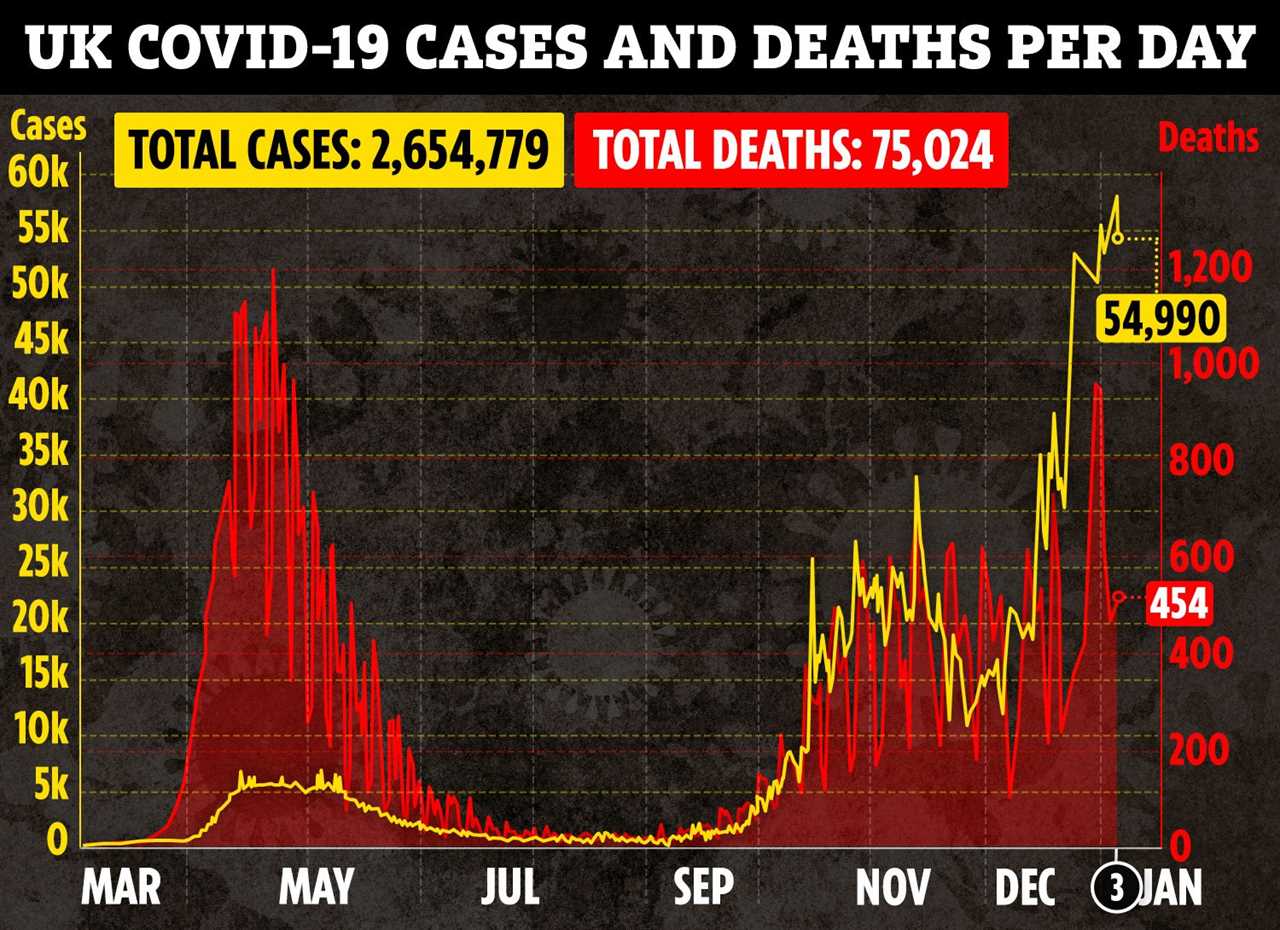
The long-awaited vaccines have created a “light at the end of the tunnel” for Brits who have been in and out of lockdowns and various tier restrictions as cases of Covid-19 continue to climb.
Health Secretary Matt Hancock said the vaccine will help Britain out of the pandemic by spring.
The UK has ordered 100 million doses of the vaccine – enough to vaccinate 50 million people.
Along with the 40 million doses of Pfizer’s vaccine, Britain now has enough doses ordered to vaccinate the entire population, Mr Hancock said.
But what Covid vaccine is best?
Experts say it’s hard to make direct comparisons when it comes to jab efficacy as it’s not clear how different pharmaceutical companies are measuring trials.
Both jabs have high efficacy rates and both require two jabs in order to give people as much protection as possible.
How effective is each jab?
Data from the Oxford/AstraZeneca team shows that the vaccine has 62.1 per cent efficacy when one dose is given – followed by another full dose.
But when people were given half a dose, followed by a full dose a month later – this shot up to 90 per cent.
The combined analysis from both dosing regimes resulted in an average efficacy of 70.4 per cent.

The Pfizer jab is 95 per cent effective.
Pfizer was the first company to complete its phase-three trial and it was found to be more than 90 per cent effective at preventing Covid-19 at the time.
A spokesperson from Pfizer said: “Although some protection from the vaccine appears to begin after the first dose (52 per cent), the information for healthcare professionals approved by the UK regulator (the MHRA) states that, individuals may not be protected until at least 7 days after their second dose of the same vaccine.
“Two doses of the vaccine 21 days apart are required to provide the maximum protection and this correlates with the level of neutralising antibodies.”
Comparing costs
The Oxford vaccine is believed to be relatively cheap to make – with estimates at around £3 per jab.
The Pfizer/BioNTech jab is more expensive and costs around £15 a jab.
Both AstraZeneca and Pfizer has said it will not sell the jab for profit – allowing it to be available to all countries.
Pfizer and BioNTech expect to be able to produce up to 50 million vaccine doses globally in 2020 and up to 1.3 billion in 2021.
The jab can also be kept at room temperature – meaning it will be easier to transport and therefor easier to roll out.
The Pfizer jab has to be kept at -70C and can only be thawed in batches of 1,000 before immunisation.
AstraZeneca said it aimed to supply millions of doses in the first quarter of next year as part of an agreement with the Government to supply up to 100 million doses.
Its chief executive Pascal Soriot said the vaccine “has been shown to be effective, well-tolerated, simple to administer and is supplied by AstraZeneca at no profit”.
How do the jabs work?
The Oxford Covid vaccine uses a harmless, weakened version of a common virus which causes a cold in chimpanzees.
Researchers have already used this technology to produce vaccines against a number of pathogens including flu, Zika and Middle East Respiratory Syndrome (Mers).
The virus is genetically modified so that it is impossible for it to grow in humans.
Scientists have transferred the genetic instructions for coronavirus’s specific “spike protein” – which it needs to invade cells – to the vaccine.
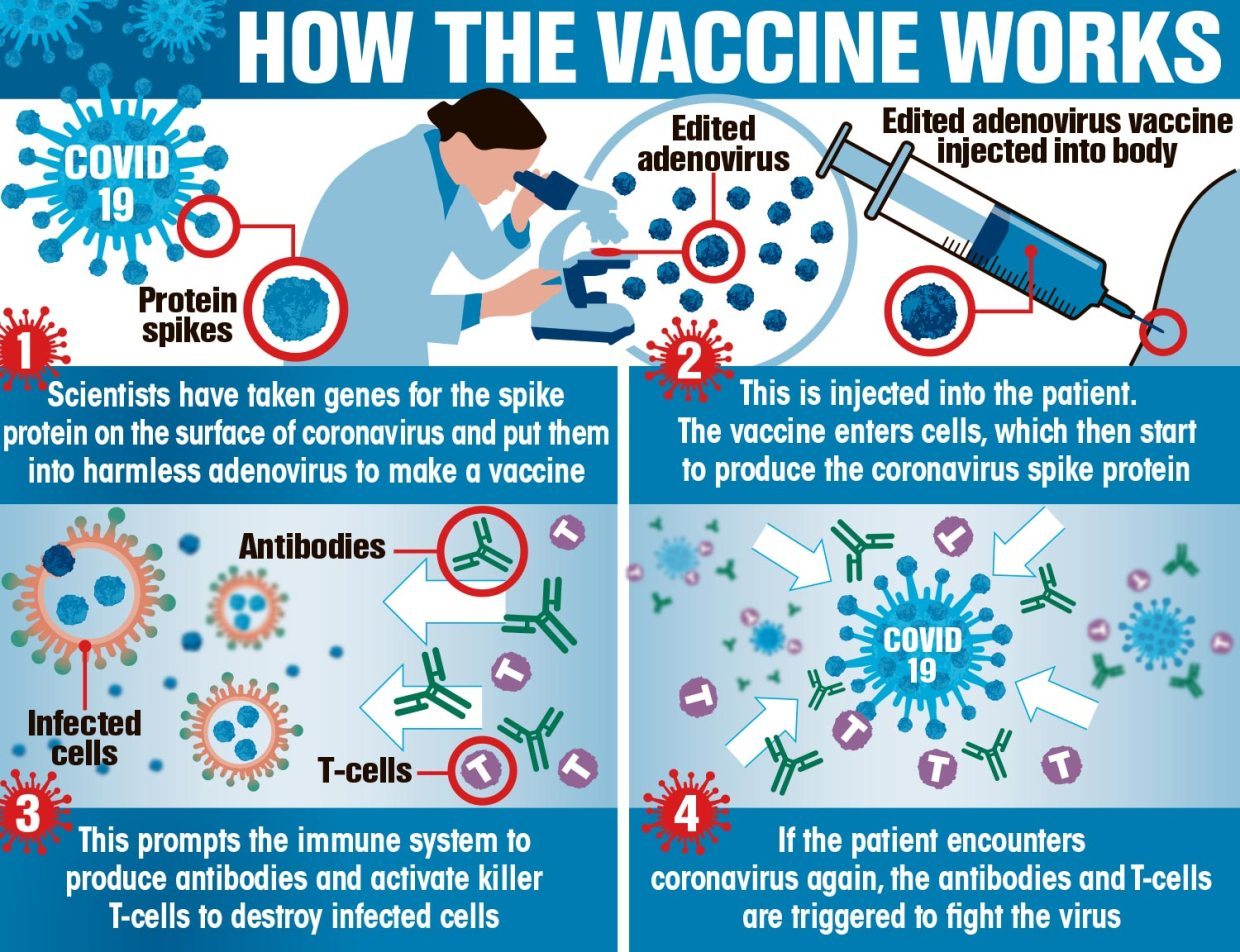
When the vaccine enters cells inside the body, it uses this genetic code to produce the surface spike protein of the coronavirus.
This induces an immune response, priming the immune system to attack coronavirus if it infects the body.
Pfizer said there had been 170 cases of the disease in its trial of more 43,000 volunteers, of which 162 were observed in the placebo arm and eight were in the vaccine group.
Ten people developed severe Covid-19, one of whom received the vaccine.
It also said the vaccine was well-tolerated and that side effects were mostly mild to moderate and cleared up quickly.
The only severe adverse event that affected more than two per cent of those vaccinated was fatigue, which affected 3.8 per cent of recipients after the second dose.
Older adults tended to report fewer and milder solicited adverse events following vaccination.
The Pfizer jab is known as a messenger vaccine (MRNA) which uses genetic code rather than a weakened form of the virus.
This is injected into the body where it enters cells – the vaccine the tells them to create antigens.
In turn the antigens are recognised by the immune system and then fight the coronavirus.






