ONE woman in the UK is diagnosed with breast cancer every 10 minutes.
It is the most common form of the disease to affect women, with around 55,000 in England developing it each year.
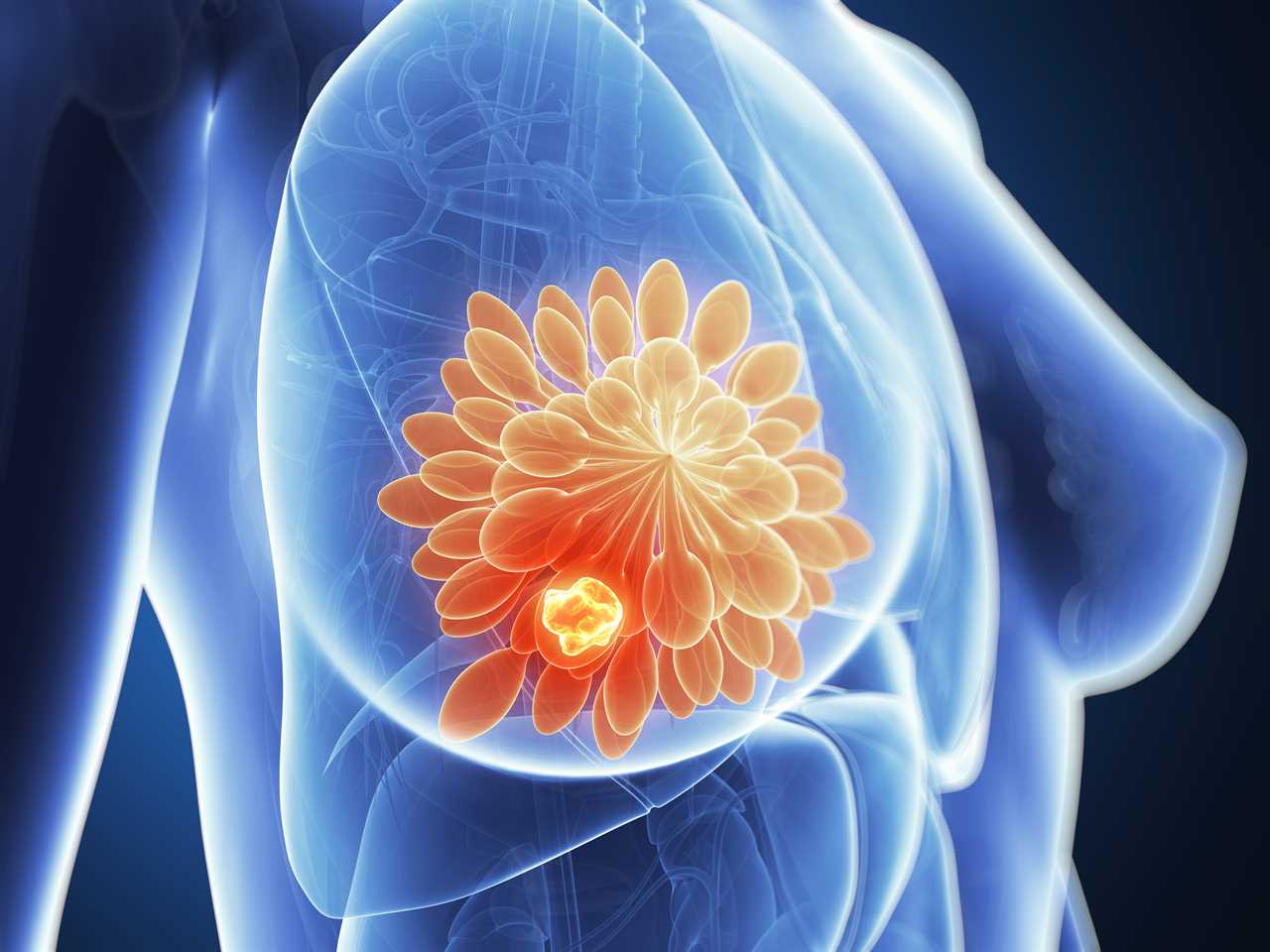
It’s important to check your breast regularly, regardless of your breast size and density, to pick up any changes sooner
Despite the disease being so wide-spread, there is a certain level of uncertainty when it comes to breast cancer symptoms.
Nuffield Health GP, Dr Unnati Desai has revealed eight of the most commonly held myths about the deadly disease and why they are in fact untrue.
1. Wearing an underwire bra increases your risk of breast cancer
“Claims that underwire bras compress the lymphatic system of the breast, thereby causing toxins to accumulate and increasing the risk of breast cancer are not backed up by science,” Dr Unnati explained.
The consensus is actually the opposite.
“The type of bra you wear, it’s tightness or your clothing has no connection to your breast cancer risk,” she explained.
2. Wearing antiperspirant increases your risk of getting breast cancer
There are claims that parabens – used as preservatives in some antiperspirants – may contribute to breast cancer development.
“However, no cause-and-effect connection between parabens and breast cancer has been established,” the expert said.
3. Smaller breast have less chance of getting breast cancer
“The risk of breast cancer occurring is not related to the size of the breasts,” the GP explained.
However, size may impact detection.
“The larger or denser the breast, the more meticulous self-examination needs to be to ensure all the deeper tissue is felt.”
“In smaller breasts, or when breast tissue density is less, changes may be more noticeable,” she said.
“It’s important to check your breast regularly, regardless of your breast size and density, to pick up any changes sooner,” she added.
4. Caffeine can cause breast cancer
“There has been no causal connection found between drinking caffeine and getting breast cancer.
“So far, it’s inconclusive whether breast soreness may be linked to caffeine,” the doctor said.
5. People with lumpy breasts (fibrocystic breast changes) more at risk of developing breast cancer
In the past, people with lumpy, dense breasts were believed to be at higher risk of getting breast cancer.
However, Dr Unnati said that science has since concluded that there is no connection after all.
“When you have these types of breasts, it can be trickier to differentiate normal tissue from cancerous tissue, so it’s important that you report any changes to your GP,” she added.
6. Breast cancer always present itself in the form of a lump
“Many people examining their breasts wrongly believe they should be looking exclusively for lumps,” the GP said.
There are other changes in the breasts to look out for, such as:
- changes to breast skin (discolouration, redness, irritation or scaliness, thickening or dimpling)
- changes to the shape or size of the breasts
- breast or nipple pain
- nipple inversion or discharge
- swelling under the armpit or around the collar bone
If you notice any change to your breast tissue, it is important to see a GP for a full assessment.
7. Mammograms expose you to so much radiation that they increase your risk of cancer
“While it’s true that radiation is used in mammography, the amount is so small that any associated risks are tiny when compared to the huge preventive benefits gained from the test,” she explained.
Mammograms can detect lumps well before they can be felt or otherwise noticed, and the earlier that lumps are caught, the better one’s chances of a positive outcome.
“The tests are not recommended in younger people as they generally have denser breast tissue, which makes it difficult to detect abnormalities.
“In this instance, the dose of radiation from a mammogram cannot be justified to warrant the use of mammograms for routine screening,” she explained.
8. All lumps are cancerous
“A lump is not necessarily a sign that you have breast cancer,” The GP explained.
Roughly 80 per cent of lumps in breasts are caused by benign (noncancerous) changes, cysts, or other conditions.
“However, if you do find a lump, it’s essential that you get it checked by a GP, just to be sure,” she added.
How to check your breasts
There is a five-step self exam you can do at home to check for any changes.
- Step one: Begin by looking in a mirror, facing it with your arms on your hips and your shoulders straight. You should be looking for any dimpling, puckering, bulging skin, redness, soreness, a rash or changes in the nipple.
- Step two: Still looking in the mirror, raise both arms above your head and check for the same changes.
- Step three: With your arms still above your head, check for any fluid coming from the nipples. This can include milky, yellow or watery fluid, or blood.
- Step four: While lying down use your opposite hand to check each breast. Using a few fingers, keeping them flat and together, go in a small circular motion around your breasts. Make sure you feel the entire breast by going top to bottom in these small circles. It helps to develop a system or pattern to make sure every inch is covered. Use light pressure for the skin and tissue just beneath, medium pressure for the tissue in the middle of your breasts, and firm pressure to feel the tissue at the back, feeling down to your ribcage.
- Step five: Feel your breasts while either standing or sitting, using the same small circular motions.






