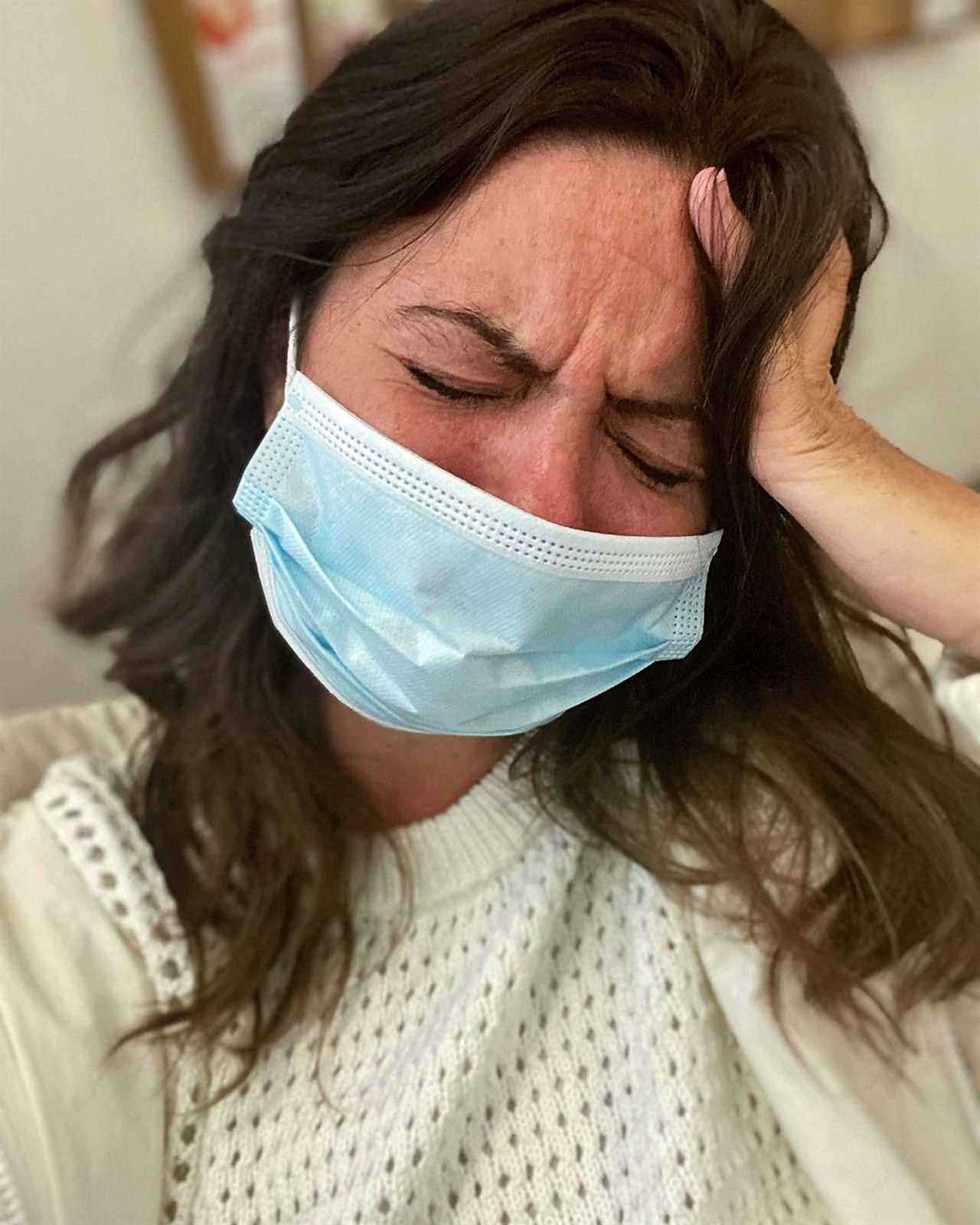
CHEMO is one of the things I love the most, yet hate in equal measure.
Right now, it’s keeping me alive.


And over the last five years it’s played a big part in helping me live to see my 40th birthday next week.
It’s a milestone doctors didn’t think possible when I was diagnosed with stage 4 bowel cancer at the age of 35.
Back then, they said I would need six cycles of treatment.
I’m fast approaching 100 cycles, and in a hideous position of knowing that in order to keep my sleeping bear cancer, well sleeping, I have to keep going.
Over the years it’s become glaringly obvious that whenever I am off treatment, be it chemo or my targeted drug therapy, my cancer grows.
It’s the cruel reality of the fact you can live longer now with stage 4 cancers, thanks to all the new drugs and targeted therapies.
But, with that comes the side effects – and the very scary and real risk that one day those options will run out and the cancer party will run riot.
While I complain about chemo, I do know I am very lucky to have it as an option right now.
Just three months ago, my body was so weak and my liver was failing – and I wasn’t strong enough to have chemo.
The issue is you can’t pump cytotoxic drugs into a failing body.
I wouldn’t have been able to process it, and I would have died anyway.
But, thanks to an emergency operation to insert a stent into my bile duct, my liver started to recover and I grew stronger.
That’s how I am still here, writing this column and looking forward to my 40th birthday next week.
Like with so many things to do with cancer, it’s all about a balance.
Weighing up the risk of nasty side effects with the risks of dying if the cancer spreads.
I’m not sure I’ve ever met anyone who finds the treatment a breeze.
It doesn’t matter how many cycles I’ve had, it doesn’t get easier.
I am writing this attached to my chemo pump again, having been vomiting violently at 3am, my husband holding my hair back, while I cuddled the toilet yet again.
Understandably, I get lots of questions about my treatment.
One common one is: “Is your chemo kinder because you still have your hair?”.
The answer is no.
I may be really lucky to still have my hair, and I do count myself very lucky on that front, but my stomach gets blitzed and I can’t feel my hands or feet due to damage to the nerves.
The treatment I am back on is known as first line chemo.