Immunotherapy Found Ineffective for Many Advanced Breast Cancers
Scientists at Stanford University have made a significant breakthrough in breast cancer treatment by identifying an "off switch" that controls the cancer's resistance to treatment and its ability to spread. Immunotherapy, which uses the body's immune system to fight cancer, is the standard course of treatment for some cancers. However, it fails to treat over 80% of advanced breast cancers. Researchers have now identified a protein called ENPP1 that acts as an on/off switch, determining whether the cancer can resist immunotherapy and metastasize.
Turning 'Cold' Tumours 'Hot'
In order for immunotherapy to be effective, T cells, a type of immune cell, need to enter the tumour. Tumours that respond to immunotherapy are known as "hot," while those that do not are called "cold" and cannot be penetrated by T cells. The researchers found that a molecule called cGAMP, produced by cancerous cells, activates an immune response that can make a tumour "hot" and responsive to immunotherapy. However, the protein ENPP1 can stop this immune response, preventing the tumour from responding to treatment.
ENPP1 Levels Determine Treatment Response
A groundbreaking breast cancer trial provided data that allowed researchers to examine the relationship between ENPP1 levels and treatment response. The results showed that patients with high ENPP1 levels had a low response to immunotherapy and a high chance of metastases. Conversely, patients with low ENPP1 levels had a high response to immunotherapy and no metastases. Mouse studies confirmed these findings, as removing ENPP1 decreased tumour growth and metastases.
Potential for Improved Treatment
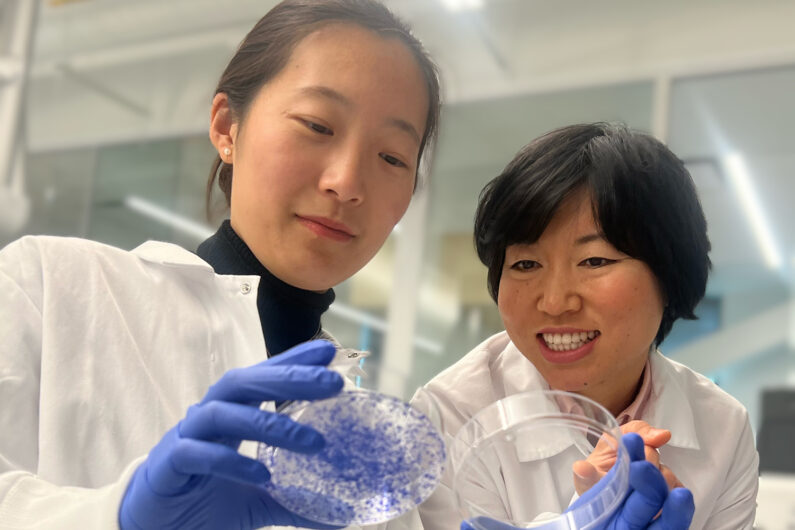
The discovery of ENPP1's role in breast cancer treatment could help clinicians determine appropriate treatment for patients. In addition, drugs that inhibit ENPP1 could enhance the effectiveness of existing therapies. Several ENPP1 inhibitors are already in clinical development. The lead researcher, Dr Lingyin Li, believes that ENPP1 may also play a critical role in treating other "cold" tumours, such as lung, pancreatic, and glioblastoma cancers.
Dr Li expressed hope that this study would inspire clinicians to investigate ENPP1's role in patient outcomes, offering hope to cancer patients.






