AI could be better at spotting dangerous breast cancer than traditional methods, researchers say.
Computers accurately predicted whether the deadly disease was likely to spread in five years from a mammogram more often.
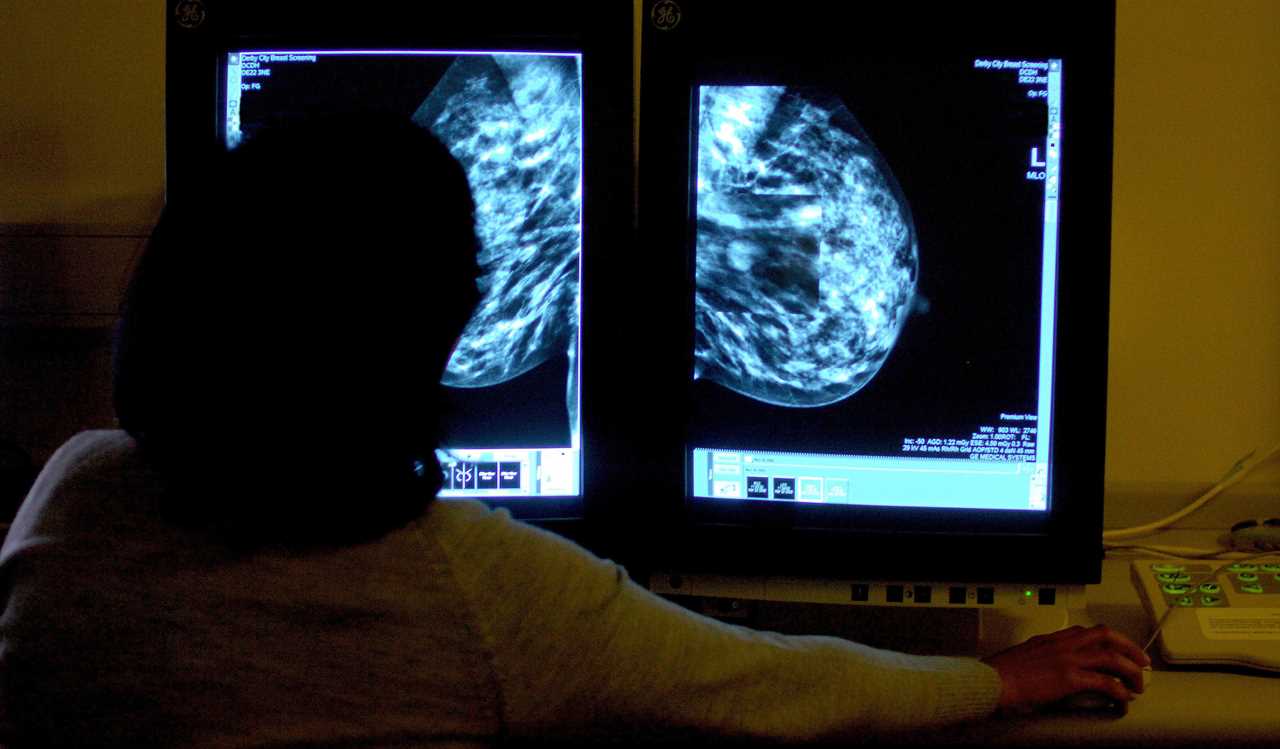
AI can predict how likely you are to develop breast cancer from mammograms better than traditional clinical models, researchers say
They were tested against standard clinical models that use information including age and family history as well as mammograms to assess women’s risk.
The AI outperformed the standard model when looking at more than 18,000 women who were screened in 2016 and tracked till 2021 — but researchers aren’t sure how exactly.
Dr Vignesh Arasu, of Kaiser Permanente Northern California, said: “AI is identifying both missed cancers and breast tissue features that help predict future cancer development.
“Something in mammograms allows us to track breast cancer risk.
“This is the ‘black box’ of AI.”
Around 55,000 women and 370 men are diagnosed with breast cancer every year in the UK.
All women aged between 50 to 71 registered with a GP are invited by the NHS for a mammogram every three years as part of a national screening programme.
If the scan reveals no sign of cancer, women are invited back to another one in three years, but clinical models can be used to predict their risk based on their age and family history.
The study, published in Radiology, looked at data from US women who had mammograms in 2016 that showed no visible evidence of cancer.
Of those, 4,584 were diagnosed with the disease within five years of the scan.
Researchers used five AI algorithms to generate cancer risk scores for within a year and from one to five years, as well as within any point over the five years.
All five of the algorithms performed better than the traditional risk model in terms of predicting their likelihood of getting breast cancer.
Dr Arasu said: “Clinical risk models depend on gathering information from different sources, which isn’t always available or collected.
“AI for cancer risk prediction offers us the opportunity to individualise every woman’s care, which isn’t systematically available.
“It’s a tool that could help us provide personalised, precision medicine on a national level.”






